Clinical Guidelines
Here you will find infomation on clinical guidelines on testing and screening. You will also find information on immunizations.
Links to Sections
Lab Checklist
Newly Arrived Immigrant Laboratory Checklist (Quick & Easy Version)
Printable Checklist PDF

Latent TB screening
Tuberculin Skin Test (PPD) if age < 2yo and Interferon Gamma Release Assay (IGRA) if age >2, though PPD acceptable if IGRA not available (IGRA preferred if history of BCG vaccine).
Immunizations
Catch-up per recommendations if no records.
CBC with Differential
Lead Testing
For all patients age 6 months to 16 years. Repeat within 3-6 months of permanent residence for children 6mo-6yo, regardless of initial result.
Intestinal Parasitic Infection
Screening (stool O&P x 2-3 samples and Strongyloides serology) or presumptive treatment per CDC guidelines with Albendazole x 1 for soil-transmitted helminths and Ivermectin x 1 for Strongyloides infection.
Be aware of contraindications to treatment.
Contraindications
Albendazole contraindications
Children < 1 year of age, pregnant women, refugees with known neurocysticercosis, evidence of cysticercosis (e.g., subcutaneous nodules), or with a history of unexplained seizures
Praziquantel contraindications
Children < 4 years of age or measuring < 94 cm, refugees with known neurocysticercosis, evidence of cysticercosis (e.g., subcutaneous nodules), or with a history of unexplained seizures.
Albendazole contraindications
Children < 1 year of age, pregnant women, refugees with known neurocysticercosis, evidence of cysticercosis (e.g., subcutaneous nodules), or with a history of unexplained seizures
Praziquantel contraindications
Children < 4 years of age or measuring < 94 cm, refugees with known neurocysticercosis, evidence of cysticercosis (e.g., subcutaneous nodules), or with a history of unexplained seizures.
Ivermectin contraindications
Children < 15 kg or measuring < 90 cm, pregnant women in any trimester or breastfeeding women within the first week after birth.
Refugee is departing from or has lived in a Loa loa endemic area Loa Loa endemic countries in Africa
Children < 15 kg or measuring < 90 cm, pregnant women in any trimester or breastfeeding women within the first week after birth.
Refugee is departing from or has lived in a Loa loa endemic area Loa Loa endemic countries in Africa

Schistosomiasis Infection
Consider presumptive treatment with Praziquantel for all immigrants from Sub-Saharan Africa per CDC guidelines. Be aware of contraindications to treatment.
Hepatitis Screening
Test for Hepatitis B if history unknown or from area with > 2% prevalence and Hepatitis C only if high-risk groups.
HIV Screening
For all ≥13 years old; for <13 years unless HIV status of mother confirmed negative and no risk factors. Consider retesting in 3 months for recent high-risk behaviors. CDC recommends 4th generation testing with antigen/antibody.
Syphilis Screening
RPR for all >15yo and for any <15yo unless maternal status clearly known and child has no risks (possible risks: unaccompanied minor, sexually active, history of sexual abuse or assault, or uncertain prior living conditions and risks).
Gonorrhea/Chlamydia Screening
Test all children at risk (unknown history, unaccompanied minor, history of sexual abuse or assault, or uncertain prior living conditions and risks), including all young adults >15 years old. Testing: GC/chlamydia NAAT from urine or from self-collected male urethral, vaginal or endocervical swabs.
Urine HCG
For all adolescents of female sex for whom consensual or non-consensual sexual activity is suspected/confirmed.
Malaria
All Sub-Saharan African immigrants within 3 months of arrival must be tested OR presumptively treated per CDC guidelines. Screen patients from all other regions only if symptomatic.
Newborn Metabolic Screen
No evidence supports universal screening. If there is concern for an inheritable metabolic condition:
MD and VA – can send up to age 6mo
DC – no maximum age but need to interpret in context of age
General Resources

Arriving Refugees
CDC Guidance for the US Domestic Medical Examination for Newly Arriving Refugees.

MN Department of Health
Interactive tool for US clinicians, which customizes screening guidance for individual refugees based on age, sex, and country of origin.

AAP Child Immigrant Health Resources
Red Book Online
Access with AAP membership.

(ACIP) Vaccine Recommendations
Persons Vaccinated Outside of the United States – Link

Policy Statement
Policy Statement: Providing Care for Children in Immigrant Families, Journal of Pediatrics, September 2019
Immunizations
If written and credible-appearing documentation present, can accept as given.
If not, vaccination or re-vaccination is standard of care (checking serologic titers is an alternative but not generally recommended for most patients).
Risks associated with giving possible extra doses of vaccines are minimal and the risks of being under- immunized are far more dangerous.

CDC Vaccination Catch-Up Schedule

CDC Recommendaitons
Full details of CDC recommendations

Office of Refugee Resettlement
Proof of Vaccines
Was patient an Unaccompanied Minor and held in the custody of the Office of Refugee Resettlement (ORR)? If so, they should have received vaccinations while in detention. Families are supposed to receive a copy of this paperwork. If not available, it can be tracked down by contacting the ORR.
Tuberculosis
CBC with Differential
Screen all newly-arrived immigrants and refugees, regardless of age and ethnicity.
Pay Attention to the Following
White blood cell count for infection
Hemoglobin/Hematocrit for anemia- high prevalence condition. Causes include Fe-deficiency, inherited anemias (hemoglobinopathies, thalassemia, enzyme defects, cell membrane defects), and infections.
RBC indices for potential causes of anemia
Eosinophilia = eosinophil > 5% or an absolute eosinophil count >400 warrants possible presumptive treatment for parasitic infection. Other causes include allergies, atopy, and medications.

Lead Testing
- For all pregnant and nursing women, in addition to prescribing a prenatal vitamin with Fe and Ca
- BLL (blood lead level) > 3.5mcg/dL is actionable (CDC lowered threshold Oct 2021)
Repeat in 6 months for all children < 6 years, regardless of initial results
- This is highest risk age group
- Disproportionate number of immigrant children live in poor housing conditions that may be contaminated with lead
- At risk for increased lead absorption with malnutrition and micronutrient deficiencies (iron, calcium, zinc)
Legislative Bill
Actions for elevated blood lead level (BLL)
Care for Refugees - Lead
Lead guidelines from CDC Domestic Guidelines for Care of Refugees
CDC: Blood Lead Levels in Children
Parasitic Infection
Hepatitis B and C
Hepatitis B (HBV)
Per CDC, all newly arriving refugees who were born in or have lived in countries with ≥2 % prevalence of chronic hepatitis B virus (HBV) infection should be tested for HBV infection.
Serologies for hepatitis B should include:
- Hepatitis B surface antigen (HBsAg)
- Hepatitis B surface antibody (anti-HBs)
- Total hepatitis B core antibody (anti-HBc)
- IgM antibody to hepatitis B core antigen (IgM anti-HBc)
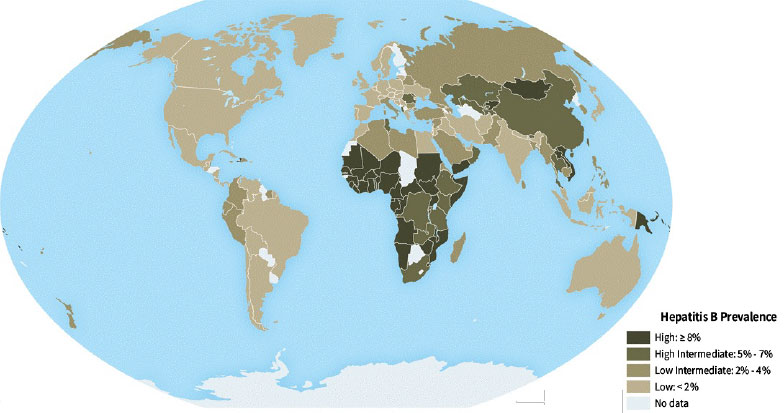
Source (map): Centers for Disease Control and Prevention. CDC Yellow Book 2020: Health Information for International Travel. New York: Oxford University Press; 2019.
Resource: Screening for Viral Hepatitis During the Domestic Medical Examination of Newly Arrived Refugees – Source
Hepatitis C (HCV)
CDC does not recommend universal HCV screening for refugee children and adolescents (< 18 years of age) with HCV antibody during the domestic medical examination unless they are members of high-risk groups, which include:
Testing: anti-HCV or HCV RNA testing.
- All children and adolescents born to HCV-positive mothers
- Unaccompanied refugee minors
- Children with risk factors including but not limited to:
- Injection and intranasal drug use (current or former)
- Chronic hemodialysis
- HIV infection
- Signs or symptoms of liver disease (e.g., abnormal liver enzyme tests, jaundice, abdominal pain or swelling, fatigue)
- Household contacts with HCV
- History of female genital mutilation or cutting (FGM/C) (data are limited

Source (map): Centers for Disease Control and Prevention. CDC Yellow Book 2020: Health Information for International Travel. New York: Oxford University Press; 2019.
Resource: Screening for Viral Hepatitis During the Domestic Medical Examination of Newly Arrived Refugees. Source
HIV Screening
- 13-64 years of age: recommend HIV screening for all patients.
- Children <13 years old: recommend screening unless HIV negative status of mother confirmed and child at low risk
- Unique risk factors for this population may include: travelling unaccompanied, history of previous known or suspected sexual activity or abuse, unstable or unsafe living condition in home country
- Medical risk factors include history of blood transfusion.
- Consider repeat screening in 3-6 months for any individual with recent exposure or high-risk activity, due to possible ‘window period’ (early infection prior to seroconversion).
- Per CDC HIV screening guidelines,
- >24mo-64yo: recommend 4th generation HIV testing (p24 Antigen/ HIV-1 and HIV-2 Antibody). This approach may identify infection up to 14 days after infection (instead of longer window period before serologic conversion with other testing methods such as oral antibody testing).
- <24mo: recommend 4th generation HIV testing. Note that a + test for HIV antibodies may reflect maternal infection. Therefore, a + HIV screen is followed up with NAT testing (DNA or RNA pcr).
- Patients and families should be clearly informed about testing and a separate consent obtained if mandated by state law.

CDC Guidelines for HIV Screening

2018 Quick Reference Guide
Recommended laboratory HIV testing algorithm for serum or plasma specimens
Syphilis Testing
- Neonates <30 days can be evaluated according to CDC guidelines
- RPR (a non-treponemal screening test) is recommended for all recent refugee/immigrants according to following approach:
- ≥15 years of age, if no overseas results are available. Note that a + screen for syphilis must be confirmed using a treponemal test.
- <15 years of age:
- who are sexually active
- who are at risk: unaccompanied, history of sexual abuse or assault, or uncertain prior living conditions and risks
- whose mother tested positive for syphilis
Highly probable congenital infection, consider when:
- abnormal exam (nonimmune hydrops, conjugated or direct hyperbilirubinemia, hepatosplenomegaly, rhinitis, skin rash, or pseudoparalysis of an extremity) OR
- serum quantitative non-treponemal (RPR) serologic titer that is 4-fold higher than the mother’s titer OR
- a positive darkfield test or PCR of lesions/body fluids
- Evaluation: CBC, LP for CSF testing, long bone radiographs
Possible congenital syphilis, consider when:
- normal exam AND titer < 4-fold mother’s titer AND mother was not treated, inadequately treated, or has no documentation of having received treatment; OR
- mother was treated with erythromycin or a regimen other than those recommended (i.e., not a penicillin G regimen); OR
- mother received recommended treatment <4 weeks before delivery.
- Evaluation: CBC, LP for CSF testing, long bone radiographs
Congenital infection less likely or unlikely:
- normal exam AND mom adequately treated before or during pregnancy.

Screening Guidelines

2021 Treatment Guidelines
Gonorrhea / Chlamydia Screening
- Consider in patients at risk, including all young adults ≥15 yo regardless of unique risk factors.
- Unique risk factors to consider for immigrant populations: travelling unaccompanied by guardian, uncertain or unsafe prior living conditions, history of any suspected sexual abuse.
- Consider testing in children with symptoms for STI.
- Consider in patients with urinalysis + for leucocyte esterase.
Test to send is GC/chlamydia NAAT from urine or from self-collected male urethral, vaginal or endocervical swabs. Screening with a rectal swab NAAT test is not routinely indicated unless symptoms of proctitis

Screening Guidelines

2021 Treatment Guidelines
Newborn Metabolic Screening
- Newborn screening should be done before birth hospital discharge if born in the United States.
- There is no evidence that universal screening is of benefit in refugee children. However, identifying inheritable metabolic conditions when there is clinical concern can be of benefit. For this reason, there is no specific maximum age limit for testing.
- Results must be interpreted within the context of age if done after first few months of life-consult with a Geneticist.
- For infants > 6mos, clinicians should perform targeted confirmatory testing (plasma amino acids, urine organic acids, acylcarnitine profile) if a metabolic disorder is suspected- consult with a Geneticist.


