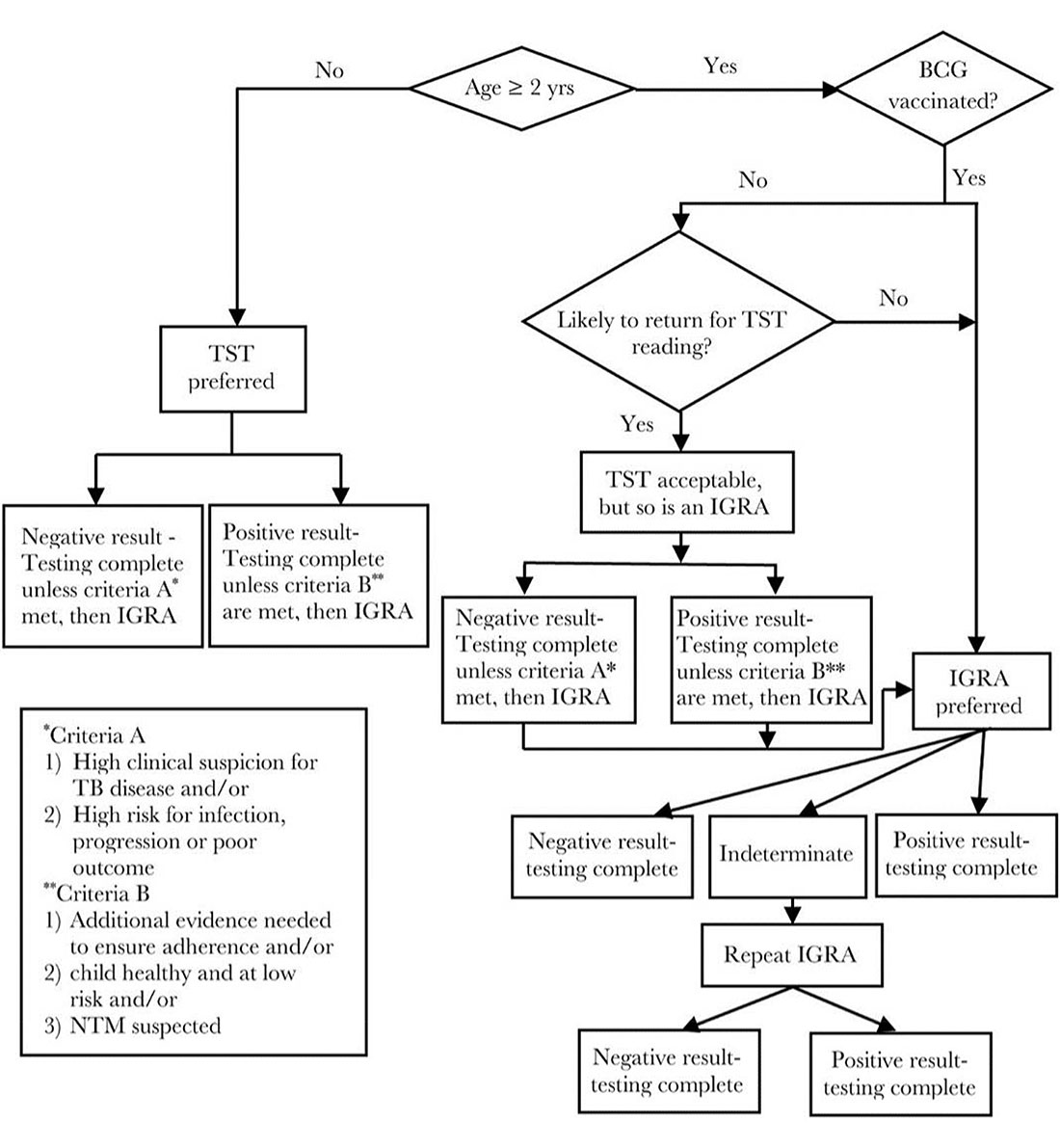
Screening
< 2 years old: PPD generally recommended; Interferon-Gamma Release Assay (IGRA) acceptable
≥ 2 years old: IGRA recommended; can place PPD if IGRA not available or feasible
If either test is positive, get CXR to rule out pulmonary TB: if CXR is clear/negative and no other signs/symptoms for active TB (cough, fever, night-sweats, weight loss, lymphadenopathy), then begin treatment for latent TB.
Key Points In Testing
- Disregard BCG vaccine status when interpreting PPD results (note: no cross-reactivity potential with IGRA testing)
- In BCG-vaccinated children, IGRA can be performed to help determine whether a “positive” TST result is attributable to LTBI or to the previous BCG vaccine when 1) additional evidence needed to ensure adherence and/or 2) child healthy and at low risk and/or 3) non tuberculosis mycobacterium suspected. (AAP Red Book)
- May consider repeating a negative TST in 6 months if chronic illness or malnutrition are present, since these conditions can potentially cause anergy (not a concern with IGRA testing since the control test results will tell you if patient is anergic)
- PPD can be placed same day as live-virus vaccine administration, but should wait > 6 weeks if placing after live-virus vaccine administration.
Algorithm for Latent TB Screening
View Chart
Risk Factors
Risk Factors for Targeted TB Screening per CDC
Tuberculin Skin Test (TST) and IGRA Recommendations for Infants, Children, and Adolescentsa. Children for whom immediate TST or IGRA is indicatedb:
- Contacts of people with confirmed or suspected contagious tuberculosis (contact investigation)
- Children with radiographic or clinical findings suggesting tuberculosis disease
- Children immigrating from countries with endemic infection (eg, Asia, Middle East, Africa, Latin America, countries of the former Soviet Union), including international adoptees
- Children with history of significantc travel to countries with endemic infection who have substantial contact with the resident populationd
Children who should have annual TST or IGRA
- Children living with HIV infection
IGRA indicates interferon-gamma release assay; HIV, human immunodeficiency virus; TBI, M tuberculosis infection.
aBacille Calmette-Guérin (BCG) immunization is not a contraindication to a TST; IGRA is generally preferred for BCG-vaccinated children. - Beginning as early as 3 months of age for TST and 2 years of age for IGRAs, for TBI and disease.
cSome experts define significant travel as birth, travel, or residence in a country with an elevated tuberculosis rate for at least 1 month. - If the child is well and has no history of exposure, the TST or IGRA should be delayed for 8 to10 weeks after return.
Red Book Online
Reference for above information.

Tuberculin Skin Test Fact Sheet
Includes interpretation of TST

Pediatrics 2021
Tuberculosis Infection in Children and Adolescents: Testing and Treatment (Clinical Report)

CDC 2020
Latent TB Infection: A Guide for Primary Health Care Providers
Treatment

TB Treatment for Children (CDC)
Recommend consulting local TB Control Program (health department).
See table and resources for medication regimen and dosage recommendations.
Treatment is recommended for children with latent TB infection to prevent them from developing TB disease. Infants, young children, and immunocompromised children with latent TB infection or children in close contact with someone with infectious TB disease, require special consideration because they are at increased risk for getting TB disease. Consultation with a pediatric TB expert is recommended before treatment begins.
Children over 2 years of age can be treated for latent TB infection with once-weekly isoniazid-rifapentine for 12 weeks. Alternative treatments for latent TB infection in children include 4 months of daily rifampin or 9 months of daily isoniazid. The regimens are equally acceptable; however, health care providers should prescribe the more convenient shorter regimens, when possible. Patients are more likely to complete shorter treatment regimens.
TB Disease Treatment for Children
TB disease in children is treated by taking several anti-TB medicines for 4, 6, or 9 months, depending on the treatment regimen. CDC does not recommend the 4-month rifapentine-moxifloxacin TB treatment regimen for children who are younger than 12 years old or have a body weight below 40 kilograms.
If a child stops taking the drugs before completion, the child can become sick again. If drugs are not taken correctly, the bacteria that are still alive may become resistant to those drugs. TB that is resistant to drugs is harder and more expensive to treat, and treatment lasts much longer (up to 18 to 24 months).

Tuberculosis Infection in Children and Adolescents
Tuberculosis Infection in Children and Adolescents: Testing and Treatment. Pediatrics December 2021

Tuberculosis Infection in Children and Adolescents
Tuberculosis (TB) remains an important problem among children in the United States and throughout the world.

